Reviewing Your Knowledge Exercise 14 Muscle Compartment Terms
Original Editors - Geoffrey De Vos
Tiptop Contributors - Delmoitie Giovanni, Scott Cornish, Geoffrey De Vos, Admin, Lucinda hampton, Kim Jackson, Glenn-Gerlo, Bettina Vansintjan, WikiSysop, Fasuba Ayobami, Karen Wilson, Wanda van Niekerk and Naomi O'Reilly
Introduction [edit | edit source]

In that location are 2 singled-out forms of compartment syndromes, acute and chronic types.
- ]Acute compartment syndrome (ACS) of the lower leg is a time-sensitive orthopedic emergency that relies heavily on precise clinical findings. Lower leg ACS is a condition in which increased pressure inside a musculus compartment surrounded by a closed fascial space leads to a pass up in tissue perfusion and compromises motor and sensory function. Key structures within the fascial compartment afflicted by increased compartment pressures include muscles, nerves and vasculature.
- Chronic exertional compartment syndrome (CECS) occurs in the setting of recurrent, reversible ischemic episodes following the cessation of activity resulting in the predictable subtract in fascial compartment pressures. Although benign, the refractory nature of CECS oftentimes results in a substantial portion of patients ultimately electing to go along with fasciotomies[i].
Prototype 1: Compartment Syndrome Picture
Late findings of ACS can pb to limb amputation, contractures, paralysis, multiorgan failure, and expiry. Authentication symptoms of ACS include the six P'southward: pain, poikilothermia, pallor, paresthesia, pulselessness, and paralysis. The definitive treatment of ACS is timely fasciotomy[2].
Etiology [edit | edit source]
Whatever condition that results in an increase of force per unit area in a compartment tin lead to the evolution of astute (ACS) or chronic exertional compartment syndrome (CECS).
ACS occurs after: [3] [iv]
- Fracture of the tibial diaphysis
- Soft-tissue injury
- Intensive muscle use
- Everyday extreme exercise activities
- Arterial injury
- Drug overdose
- Burns
CECS occurs later:
- Repetitive and strenuous exercise. During strenuous exercise, at that place can be upwards to a 20% increment in muscle volume and weight due to increased claret flow and oedema, so pressure increases. If this pressure elevates to xxx mmHg or more than, small vessels in the tissue become compressed, which leads to reduced food blood menstruation, ischemia and pain.[5] [ [6] The inductive compartment is affected more than frequently than the lateral, deep and superficial posterior compartments.[7]
Epidemiolgy [edit | edit source]
Chronic exertional compartment syndrome is typically considered a rare crusade of lower extremity pain, with a reported incidence charge per unit in active patients presenting with exercise-induced leg hurting to exist 33%[1]
Male patients are ten times more than impacted by ACS than females, possibly due to males having larger muscle mass within a fixed compartment.
Younger patients (≤ 35 years of age) are also at a greater risk to ACS due to having tighter fascia and larger muscle mass and as they are prone to injuries or accidents[ii]
Clinically Relevant Anatomy [edit | edit source]
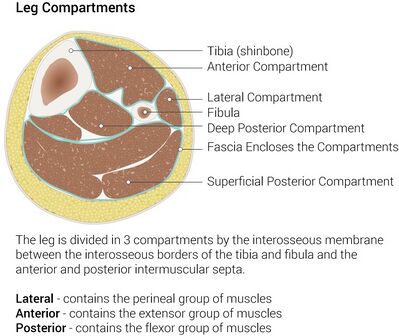
In that location are 4 compartments in the lower leg and these include the anterior, lateral, superficial posterior and deep posterior compartments.
Each compartment contains specific nerves, arteries and veins, muscles, and bony structures that with injury contribute to the unique clinical presentations in ACS.
Cognition virtually the most important structures within these compartments is critical to efficiently assess and diagnose physiologic changes in ACS that contribute to pathologic development[2]
Prototype 2: Leg compartments lower limb
Characteristics/Clinical Presentation [edit | edit source]
Patients with compartment syndrome of the lower leg suffer from long term impairment such equally reduced muscular strength, reduced range of motion and pain. [8] The most mutual symptoms by a compartment syndrome are:[4]
- Feeling of tightness
- Swelling
- Pain (on active flexion knee and particularly passive stretching of the muscles)
- Paresthesia
Diagnostic Procedures [edit | edit source]
Diagnosis of ACS is based largely on physical examination and six cardinal clinical manifestations described as the six P's.
- The half-dozen P'due south include: Pain, Poikilothermia (disability to regulate one's body temperature), Paresthesia, Paralysis, Pulselessness, and Pallor.
- The earliest indicator of developing ACS is severe pain.
- Pulselessness, paresthesia, and complete paralysis are constitute in the belatedly stage of ACS.
- Additionally, series measurement of ICP is disquisitional in confirming and determine progression of ACS.
- Other diagnostic considerations including the use of ancillary testing such as laboratory testing or imaging.
Cess [edit | edit source]
Acute compartment syndrome
- On assessment, the master finding is swelling of the afflicted extremity
- The inability to actively movement flexors and extensors of the human foot is an of import indicator [v]
- Signs such equally progression of pain
- Pain with passive stretching of the affected muscles
- Often a disturbance awareness in the web space betwixt the first and second toes is found as a consequence of compression or ischemia of the deep peroneal nerve. This nervus is found in the inductive compartment. Reduced sensation represents a late sign of ACS
- Absence of arterial pulse is more often a sign of arterial injury than a tardily sign of ACS
Chronic exertional compartment syndrome
- Pain starts within first 30 minutes of exercise and tin radiate to ankle/human foot [6]
- Pain ceases when action is stopped
- Daily activities usually non provocative
- On assessment, the chief finding is swelling of the afflicted extremity
- The inability to actively move flexors and extensors of the foot is an important indicator
- Signs such equally progression of pain
- Recording of intra-compartmental tissue pressures [6] [9] (needle and manometer, wick catheter, slit catheter)
Treatment [edit | edit source]

The gilt standard treatment is fasciotomy, but well-nigh of the reports on its effectiveness are in brusk follow-up periods.[10]
Image three: Compartment syndrome with fasciotomy procedure
Nonoperative treatment
- Whenever safe and possible, uncomplicated treatment measure in ACS include loosening ace wraps, compression dressings, splints and uni- or bivalving casts.
- Summit of extremity no college than the level of the heart facilitates venous drainage, reduces edema and maximize tissue perfusion.
- Further, avoidance of knee flexion and human foot dorsiflexion will facilitate uncompromised circulation throughout a limb and limit increases in ICP in the deep posterior compartment respectively[2]
CECS is typically managed nonoperatively for a one- to iii-month elapsing, and surgical direction may often be delayed and/or electively performed after having a discussion with the patient (or athlete) regarding the ideal timing given the athletes current sport-specific requirements.
Conservative management consists of residue, activity modification, stretching, orthotics, and concrete therapy. Nonoperative modalities include, but are not express to:
- NSAIDs
- Botulinum toxin injections[ii]
- Gait grooming
Concrete Therapy Management [edit | edit source]
The just nonoperative treatment that is certain to convalesce the pain of CECS is the abeyance of causative activities.
- Normal physical activities should be modified, hurting allowing.
- Cycling may be substituted for running in patients who wish to maintain their cardiorespiratory fettle, as it is associated with a lower risk of compartment force per unit area elevation.
- Massage therapy may provide some benefit to patients with balmy symptoms or to those who turn down surgical intervention.
Overall, however, nonoperative handling has been more often than not unsuccessful [6] and symptoms will not disappear without handling.
Concrete Therapy in CECS
Conservative therapy has been attempted for CECS, just it is generally unsuccessful. Symptoms typically recur once the patient returns to exercise. Discontinuing participation in sports is an option, just it is a choice that most athletes refuse. [eleven]
Pre-surgical therapy
Pre-surgical therapy in CECS includes reduction of activity, with encouragement of cross-training and musculus stretching earlier initiating exercise. Other preoperative measures are rest, shoe modification, and the use of nonsteroidal anti-inflammatory medications (NSAIDs) to reduce inflammation.[11]
Post-surgical therapy
Post-surgical therapy for CECS includes assisted weight bearing with some variation, depending on surgical technique. Early mobilisation is recommended equally soon every bit possible to minimise scarring, which can lead to adhesions and a recurrence of the syndrome.
Activity can exist upgraded to stationary cycling and swimming later on healing of the surgical wounds. Isokinetic muscle strengthening exercises tin can brainstorm at 3-4 weeks. Running is integrated into the activity program at iii-vi weeks. Full activeness is introduced at approximately 6-12 weeks, with a focus on speed and agility.[11] The post-obit are recommendations for a full recovery and to avert recurrence;
- Wearing more than appropriate footwear to the terrain
- Choosing more than appropriate surfaces and terrain for exercise
- Pacing your activities
- Avoiding certain activities altogether
- Mastering strategies for recovery and maintenance of good health (e.g, appropriate rest betwixt sessions)
- Modifying the workplace to lower the risk of injury
Postoperative physical therapy is essential for a successful recovery. depending on the nature of the procedure, expected timelines for healing and progress made during rehabilitation. Handling incorporates strategies to restore range of motion, mobility, strength and function.[12]
Conclusion [edit | edit source]
- Acute Compartment Syndrome (ACS) of the lower leg is a time sensitive limb threatening surgical emergency.
- Tardily findings of ACS tin can pb to limb amputation, contractures, paralysis, multi-organ failure and death.
- Diagnosis is based on clinical suspicion, cess of the vi P's (hurting, poikilothermia, pallor, paresthesia, pulselessness and paralysis) and intracompartmental pressure (ICP).
- ICP measurement above 30mmHg is considered critical and treatment with emergent surgical decompression should exist considered.
- The gilded standard of acute compartment handling is full fasciotomy[2].
References [edit | edit source]
- ↑ 1.0 one.1 Chandwani D, Varacallo M. Exertional compartment syndrome. InStatPearls [Internet] 2020 Jun 3. StatPearls Publishing. Bachelor: https://www.statpearls.com/articlelibrary/viewarticle/64490/(accessed 29.10.2021)
- ↑ 2.0 two.ane ii.2 2.3 two.4 ii.five Pechar J, Lyons MM. Acute compartment syndrome of the lower leg: a review. The Journal for Nurse Practitioners. 2016 Apr 1;12(four):265-70. Available: https://world wide web.ncbi.nlm.nih.gov/pmc/articles/PMC4970751/(accessed 29.10.2021)
- ↑ McQueen, One thousand. K., and P. Gaston. "Acute compartment syndrome." Bone & Articulation Periodical 82.2 (2000): 200-203.
- ↑ 4.0 4.1 Abraham TR. Acute Compartment Syndrome. Physical Medicine and Rehabilitation. (2016)
- ↑ v.0 5.1 Oprel PP., Eversdij MG., Vlot J., Tuinebreijer WE. The Acute Compartment Syndrome of the Lower Leg: A Hard Diagnosis? Department of Surgery-Traumatology and Pediatric Surgery, Erasmus MC, University Medical Eye Rotterdam, The Open Orthopaedics Periodical, 2010, 4, 115-119
- ↑ 6.0 6.1 vi.ii 6.iii Bong MR., Polatsch DB., Jazrawi LM., Rokit Equally. Chronic Exertional Compartment Syndrome, Diagnosis and Management. Infirmary for Joint Diseases 2005, Volume 62, Numbers 3 & iv.
- ↑ Van der Wal, West. A., et al. "The natural course of chronic exertional compartment syndrome of the lower leg." Knee Surgery, Sports Traumatology, Arthroscopy 23.vii (2015): 2136-2141.
- ↑ Frink, Michael, et al. "Long term results of compartment syndrome of the lower limb in polytraumatised patients." Injury 38.5 (2007): 607-613
- ↑ Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH: Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med 1990;18:35-40.
- ↑ Chechik, O., M. Rachevsky, and G. Morag. "Michael Drexler, T. Frenkel Rutenberg, Due north. Rozen, Y. Warschawski, E. Rath, Unmarried minimal incision fasciotomy for the treatment of chronic exertional compartment syndrome: outcomes and complications, Archives of Orthopaedic and Trauma Surgery · September 2016
- ↑ 11.0 11.1 11.two Gregory A Rowdon, Medico; Chief Editor: Craig C Young, MD et al Chronic Exertional Compartment Syndrome Handling & Management Updated: Oct 08, 2015.
- ↑ Val Irion, Robert A. Magnussen, Timothy 50. Miller , Christopher C. Kaeding "Return to activity following fasciotomy for chronic exertional compartment syndrome" Eur J Orthop Surg Traumatol , Volume 24, Upshot vii, pp 1223–1228.
kellybarigoinathe.blogspot.com
Source: https://www.physio-pedia.com/Compartment_Syndrome_of_the_Lower_Leg
0 Response to "Reviewing Your Knowledge Exercise 14 Muscle Compartment Terms"
Post a Comment